Abstract
In late December 2019, a cluster of pneumonia cases of unknown aetiology linked to a market was reported in Wuhan, China1. The causative agent was identified as the coronavirus species related to severe acute respiratory syndrome and was named SARS-CoV-2 (ref. 2). By April 16, the virus had spread to 185 different countries, infected more than 2,000,000 people and caused more than 130,000 deaths3. In the Netherlands, the first case of SARS-CoV-2 was reported on February 27. The outbreak started with several different introductory events from Italy, Austria, Germany and France, followed by a local amplification in the south of the Netherlands and later also outside of it.
The combination of whole-genome sequence analysis and near-real-time epidemiology resulted in reliable assessments of the extent of SARS-CoV-2 transmission in the community, facilitating early decision-making to control local transmission. of SARS-CoV-2 in the community. The Netherlands. We demonstrate how this data was generated and analyzed, and how SARS-CoV-2 whole-genome sequencing, in combination with epidemiological data, was used to inform public health decision-making in the Netherlands.
Methods
- Response to COVID-19
This study was carried out in collaboration with the national outbreak response team. This team develops a guide on case detection and containment, based on recommendations and expert advice from WHO and the European Center for Disease Prevention and Control, as defined by the crisis and emergency response structure. Initially, diagnoses were made in suspected cases with a history of recent travel to China, but between February 25 and 28, suspected cases with a history of travel to affected municipalities in northern Italy were also analyzed.
Between March 1 and 11, all suspected cases with a history of travel to the four northern Italian provinces were analyzed, and after March 11, all suspected cases with a history of travel to Italy were analyzed. The sequencing effort was incorporated into the gradual response to the outbreak which evolved from the initial testing of symptomatic travellers, including testing of symptomatic contacts (phase 1), followed by the inclusion of routine testing of hospitalized patients with severe respiratory infections (phase 2), up to the inclusion of healthcare workers with a low-threshold case definition and tests to define the scope of suspect groups (phase 3).
Depending on the phase and clinical severity, initial contact with patients was established through public health doctors or nurses from the municipal health service (for cases related to travel, case contacts (hospitalized) and patients belonging to risk groups ). The different phases of this study were based on the observations described in this manuscript. Ethical approval was not required for this study as only anonymous aggregated data was used and no human medical interventions were performed.
- Contact tracing
On January 29, COVID-19 was classified as a notifiable disease in group A in the Netherlands, and doctors and laboratories had to report any suspected and confirmed cases by phone to the Dutch public health services (PHS). Upon notification, PHS initiates source identification and contact tracing and conducts risk assessments.
In the early phase of the outbreak (containment), the PHS tracked and informed all contacts of high- and low-risk cases with the goal of stopping further transmission. Epidemiological information such as demographic data, symptoms, symptom onset date, travel history, contact details, suspected source, underlying disease, and occupation was recorded for each case. People were asked to report their travel history for the past 14 days, including possible trips to multiple countries.
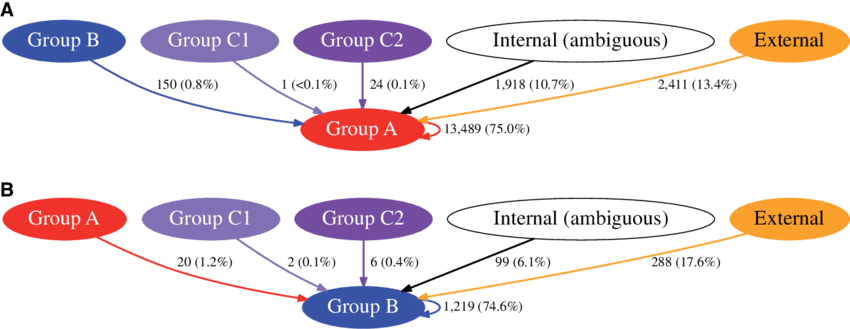
Due to the magnitude of the COVID-19 outbreak, this quickly became impractical in severely affected regions, and the strategy shifted to only recording data on confirmed cases and informing their high-risk contacts (phase 2) with a continuous active search for cases in fewer affected regions. The PHS informed the Netherlands National Public Health Authority (RIVM) of all laboratory-confirmed cases. There a national registry of cases was kept in which a contact matrix of the first 250 cases was kept.
- Selection of samples
In the first phase, all samples were selected for sequencing, reflecting cases associated with travel and their contacts. In the second phase, priority was given to patients identified through improved case finding by testing hospitalized patients with severe acute respiratory infections and continuous sequencing of new incursions. In the third phase, the epidemic began to expand exponentially and sequencing was carried out to continue monitoring the evolution of the outbreak. According to the national testing policy, a substantial proportion of the newly sequenced cases were healthcare workers (20%).
- SARS-CoV-2 diagnosis
Clinical samples were collected and phocine distemper virus was added as an internal nucleic acid extraction control (NA) to the supernatant. Clinical samples included oropharyngeal and nasopharyngeal swabs, bronchoalveolar lavage, and sputum. Total NA was extracted from the supernatant using Roche MagNA Pure systems. NA was screened for the presence of SARS-CoV-2 using real-time single-complex reverse-transcription PCR for the phocine distemper virus, for the SARS-CoV-2 RdRp gene, and for the SARS E gene. -CoV-2 as described by Corman et al.